
Not only does noncompliance lead to fines, sanctions, and accreditation issues, it also does lasting damage to an organization’s reputation and brand. Automating accounts receivable processes is the surest way to avoid compliance errors involving data Accounting Errors privacy, invoicing practices, accounting fraud, and other key areas of concern. Patients need to know that their healthcare provider can be trusted not only with their health, but also their payments and privacy. Accounts receivable refers to the unpaid invoices that patients, insurance companies, or third-party payers owe healthcare providers for services rendered.
Unlocking Efficiency in Patient Care: The Power of Accounts Receivable Logs
Claim denials, where the insurer refuses to pay for the service rendered, can lead to an increase in AR and potential bad debt. These unique challenges necessitate specialized AR strategies in medical practices. Managing AR effectively can also minimize instances of bad debt, which occurs when payment for services becomes highly unlikely or impossible to collect. It’s important for medical practices to keep a close eye on their AR and adopt strategies to manage it efficiently.

Collecting Bad Debt
Secondly, physicians, healthcare organization leaders, administrators, and front office staff need strong leadership qualities to educate and inform all patients. Healthcare IT companies can increase revenue and promote a practice’s staff members’ leadership qualities by prioritizing training for staff and educating their patients. Delays in claim adjudication, denials, or underpayments can lead to outstanding balances. Practices must work closely with payers to resolve issues and ensure timely reimbursement. Automation tools, such as revenue cycle management (RCM) platforms, can streamline claim submission, track outstanding balances, and provide real-time insights into accounts receivable. Challenges include collecting timely payments, managing bad debt, dealing with insurance claim denials, and handling outstanding balances.
- Managing AR effectively can also minimize instances of bad debt, which occurs when payment for services becomes highly unlikely or impossible to collect.
- With customizable templates and settings, you can tailor your dunning letters to align with your brand and effectively communicate with customers regarding outstanding balances.
- This increases the pressure on healthcare organizations to follow up on denied or appealed claims.
- The first piece of advice is to not resubmit a claim for payment unless there is proof the initial claim was never received.
Understanding Accounts Receivable (AR) for Medical Practices
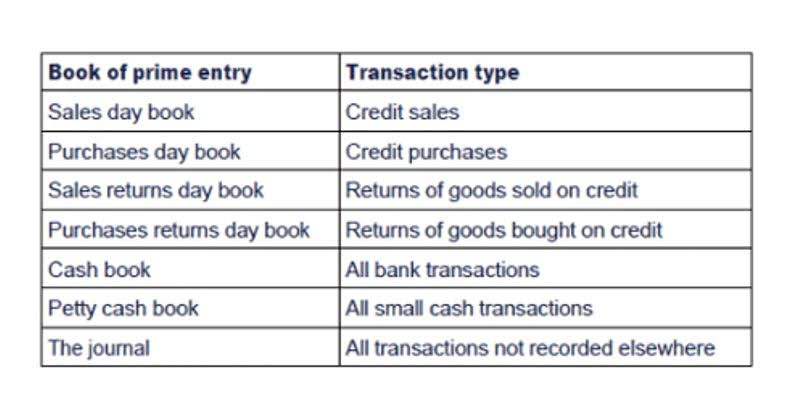
Dunning letters are communication tools that remind customers or clients about overdue payments. With customizable templates and settings, you can tailor your dunning petty cash letters to align with your brand and effectively communicate with customers regarding outstanding balances. Automated reminders and notifications can be programmed into the account receivable log to ensure that healthcare providers are aware of impending deadlines, outstanding payments, or potential issues.
- In conclusion, an effective accounts receivable log plays a vital role in managing patient accounts, improving cash flow management, enhancing patient communication, and reducing administrative burdens.
- By putting best practices into effect, healthcare businesses can drastically cut down on AR days and increase revenue cycle efficiency.
- Providers can better plan their budgets and direct resources where they are most needed by cutting down on the number of days outstanding.
- The payer’s process involves easily completed forms, including methods to submit multiple claims at one time.
- Another best practice is always providing financial assistance program information if needed.
- Nowadays we observed that various factors that cause overheads for healthcare organizations such as outstanding claims and delayed collections as well as stringent federal regulations.
One often overlooked yet vital aspect of this process is the accounts receivable log for individual patients. A well-organized and up-to-date account receivable log serves as a vital tool in tracking outstanding payments, identifying potential issues, and ensuring timely follow-ups with patients. It matters because it reduces the risk of revenue gaps by increasing financial stability. Furthermore, patient accounts receivable management enables providers to streamline the billing process. Hence, clear communication with patients regarding their outstanding payment enhances patient experience and trust.
Saving Time: Practice Innovation Boot Camp

It also makes organizations more reliable and environmentally friendly, as patient data is stored and updated on the cloud. Keeping up with the latest technology should always be a goal for accounts receivable. Smoothly integrating new tech and training employees on how to use it effectively is vital to keeping payments flowing as they should. Gathering patient information such as payment needs sets up both patient interactions and billing transactions for success moving forward.
- The approach allows the provider to focus their efforts on who is most likely to pay and who can afford to pay.
- These difficulties highlight the necessity of an organized AR management procedure supported by technology and qualified experts.
- Medicare Advantage plans have an escalation process like Medicare and can often be handled through online submission.
- You may find, however, that you still have low collection rates with this option.
- As a result, internal personnel may concentrate on providing patient care rather than handling paperwork.
- Challenges include collecting timely payments, managing bad debt, dealing with insurance claim denials, and handling outstanding balances.
The majority of providers strive to maintain Days in Accounts Receivable (DAR) below 50, while industry standards can differ. Paying employees, covering operating expenses, and investing in improved patient care technologies are all made possible by accounts receivable log for individual patients prompt reimbursement. Work to decrease claims that don’t pay because the patient’s deductible was not yet met.
The Role of a Dedicated AR Team or Billing Service
If a hospital can manage its A/R system properly, it will receive the revenue it needs to stay open and treat more patients. For pharmacies with delivery services, A/R accounts prove invaluable for billing patients on a monthly basis. This feature simplifies the payment process, making it more convenient for both the pharmacy and the patients. The trouble is, you can’t expect to be efficient in collecting on accounts receivable if you don’t have a prioritization method in place with your team, and making a plan isn’t always easy. Team MHC consists of a multitude of roles, functions, and expertise within MHC.

Collections are best handled by trained personnel familiar with collection regulations. Documentation affects cash flow for both emergency and non-emergency services. The best thing emergency providers can do is to document how they were dispatched. This information helps billing determine if the call was ALS or BLS, thereby affecting reimbursement. When done appropriately, the billing is done cleanly and accounts receivable does not grow.
+ There are no comments
Add yours